Gastroparesis is a chronic digestive condition where the stomach cannot empty itself of food in a normal fashion due to weakened muscular contractions. Often referred to as delayed gastric emptying, this disorder prevents the stomach …
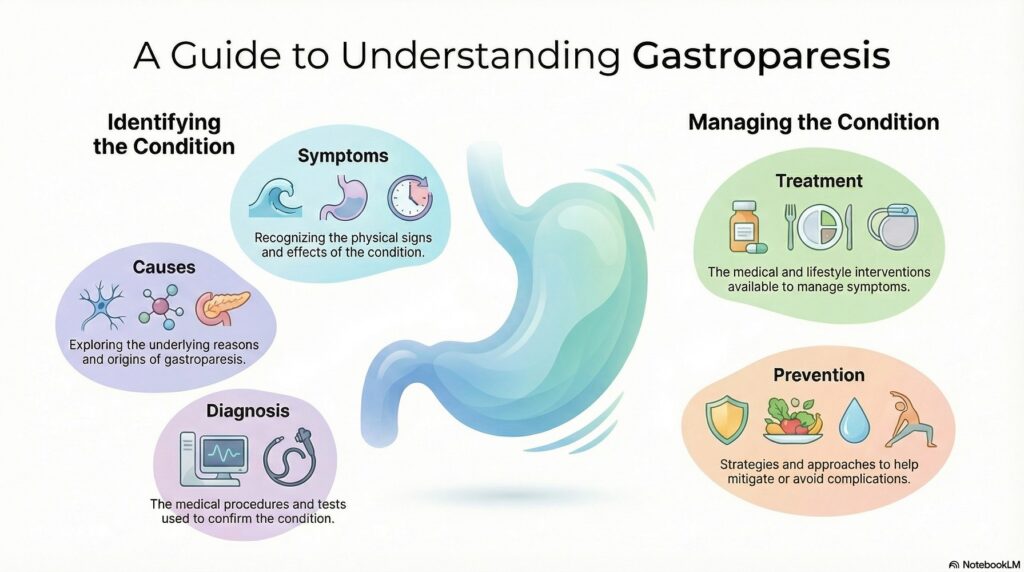
Gastroparesis – Symptoms, Causes, Diagnosis, Treatment & Prevention
Gastroparesis is a chronic digestive condition where the stomach cannot empty itself of food in a normal fashion due to weakened muscular contractions. Often referred to as delayed gastric emptying, this disorder prevents the stomach from properly processing food and moving it into the small intestine.
Common Symptoms of Gastroparesis
The most frequently reported symptom of gastroparesis is nausea, which affects nearly 96% of patients. Many individuals experience a sensation of fullness shortly after starting a meal, even after only a few bites. Other significant signs include:
Chronic vomiting, sometimes of undigested food eaten hours prior.
Abdominal bloating and upper abdominal pain.
Excessive belching and persistent heartburn.
Unintended weight loss and poor appetite due to malnutrition.
Primary Causes of Gastroparesis
Damage to the vagus nerve, which controls the stomach muscles, is the primary underlying cause of gastroparesis. When this nerve is damaged, the muscles of the stomach do not function correctly, causing food to sit in the stomach for too long. Major contributing factors include:
Diabetes: Approximately 30% of cases are linked to Type 1 or Type 2 diabetes, which can cause nerve damage over time.
Post-Viral Infection: Infections from viruses like norovirus or rotavirus can trigger the onset of the condition.
Surgery: Complications from surgeries on the stomach or digestive organs can inadvertently damage the vagus nerve.
Medications: Narcotics, certain antidepressants, and calcium channel blockers can slow gastric emptying.
Diagnostic Procedures of Gastroparesis
Healthcare providers typically use specialized tests to confirm a diagnosis and rule out blockages. The most common “gold standard” test is a gastric emptying study, where a patient eats a meal containing a small amount of radioactive material to track how quickly it leaves the stomach. Doctors may also perform an upper endoscopy to visualize the stomach lining or use an ultrasound to rule out gallbladder or kidney issues.
Treatment and Management of Gastroparesis
While there is currently no cure for gastroparesis, treatments focus on managing symptoms and maintaining nutrition. Management strategies often include a combination of dietary changes, such as eating smaller, more frequent meals that are low in fiber and fat.
Prevention and Risk Reduction
Preventing gastroparesis primarily involves managing underlying health conditions that damage the nervous system. For individuals with diabetes, maintaining strict control over blood sugar levels is the most effective way to reduce the risk of developing the condition. Additionally, avoiding medications known to slow digestion and seeking prompt treatment for viral gastrointestinal infections may help mitigate long-term complications.
Read more: Gastroenterologists near me | Why does Knee Replacement Surgery Fails